Piriformis weak leg issues can add additional suffering on top of pain and other agonizing symptoms. Weakness is often a result of sciatic nerve compression that is caused by the piriformis muscle and typically diagnosed as piriformis syndrome. However, perceptions of weakness may also occur in conjunction with piriformis injury, as well.
Weakness comes in both objective and subjective forms. Objective weakness describes symptoms wherein a muscular deficit can be verified by neurological testing. Meanwhile, subjective weakness involves feelings of decreased physical ability in the leg without verified reduction in strength. Both types of leg weakness can be created by the piriformis muscle, but subjective varieties are more common when discussing piriformis injury, while piriformis syndrome can produce either variation of symptomology.
This discussion investigates how weakness in one or both legs might be related to the piriformis muscle. We will explore the possibility of symptoms being created by piriformis syndrome, as well as localized piriformis trauma.
Piriformis Weak Leg Symptoms
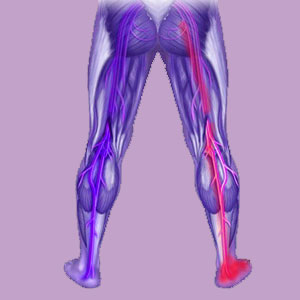
Weakness in the leg might be expressed high up in the region where the leg connects to the body or anywhere below this level, all the way down to the foot. Weakness in the high areas of the leg and hip are usually subjective and due to injury in the piriformis or one or more of the related tissues of the lateral rotator group. Meanwhile, widespread or lower leg weakness can be objective or subjective and is usually the result of piriformis compression of the sciatic nerve.
Weakness might cause patients to lose some or all of the ability to perform strenuous physical activities with their legs, including running or sports participation. In rare cases of severe weakness, patients might have difficulty ambulating or even standing under their own power. Some patients may also demonstrate related innervation dysfunctions, such as dorsiflexion deficit, more often diagnosed as foot drop.
Piriformis Syndrome Weakness
Piriformis syndrome can create innervation problems throughout the lower body anatomy due to compression of the major source of nerve signals in the legs: the sciatic nerve. Although pain is traditionally thought to be a result of chronic neurological compression, scientific evidence tells that lasting compression of any nerve will cause pain to fade and numbness and weakness to become the primary symptomatic complaints. Therefore, it is logical that patients who are suffering true compression of the sciatic nerve due to piriformis muscle spasms will experience weakness and possible numbness of objective variety after some time.
Weakness in the legs might affect any region from the lower buttocks down and might be focally present in some areas or widespread throughout the entire leg and/or foot or just certain areas of the leg or foot. Patients might also suffer related compression of the pudendal nerve, causing similar weakness and numbness expressions in the pelvis, perineum, groin and even in the genitals themselves.
Piriformis Weak Leg Injury
Injury, RSI or overexertion of the piriformis muscle can create transient weakness in the upper leg, especially when the patient attempts to perform some variety of exercise with the hip region. The entire leg often feels weak, with focal regions of deficient strength and possibly pain in and around the substance of the muscle itself. Many patients report this as hip pain or sacroiliac pain, since these structures are in the exact same vicinity anatomically.
Weakness in relation to piriformis injury should resolve as the body heals the trauma. Depending on the exact nature and severity of the damage, weakness and associated pain might endure for several days to several weeks while steadily improving day by day.
Chronic pain and weakness that result from injury might require physical therapy or may indicate a more significant type of trauma than first identified. Some patients may suffer tissue detachments that may require surgical intervention to correct. However, in most cases where weakness persists despite time and treatment, the diagnosis turns out to be wrong and the actual origin of symptoms is some other structural or nonstructural source, such as regional ischemia.